- Jul 08, 2025
- By TJICLondon
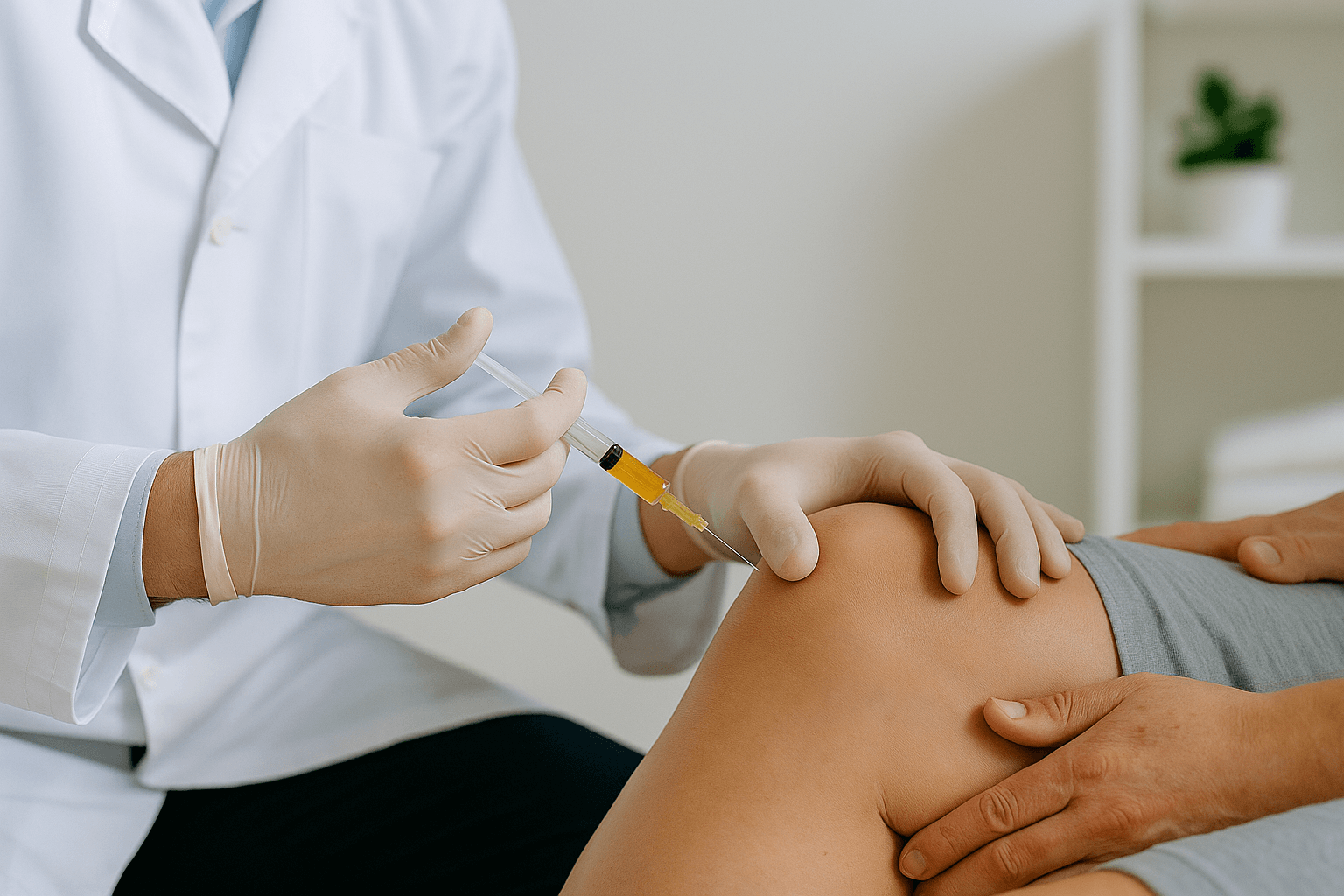
The Benefits of Ultrasound-Guided Injections for Joint Pain
Joint pain can significantly impact one’s quality of life, and many people turn to injection therapies (like corticosteroid or gel injections) for relief. In recent years, ultrasound-guided injections have become a game changer in treating joint pain. Instead of performing injections “blind” (by feel or anatomical landmarks alone), doctors now use ultrasound imaging to see exactly where the needle is going in real time. This innovation has revolutionized how injections are performed, offering many advantages over the old blind approach . Below, we explore what ultrasound-guided injections are, their accuracy and safety benefits, how they improve outcomes, which conditions benefit most, and what patients can expect during the procedure. (Hint: if you’re in London and struggling with joint pain, this high-tech option is likely available at clinics near you.)
What Are Ultrasound-Guided Injections? (How the Procedure Works)
Ultrasound-guided injections are simply injections performed with the aid of ultrasound imaging. Ultrasound is a safe imaging technology that uses high-frequency sound waves (and no radiation) to produce live pictures of the inside of your body. During an ultrasound-guided injection, a doctor uses an ultrasound probe on the skin to visualize the tissues and the target joint on a monitor. This allows the physician to precisely guide the needle to the intended spot while watching its path in real time. In other words, the ultrasound acts like a GPS for the needle, helping navigate to the exact location of pain or injury. The procedure itself still involves the typical steps of an injection – cleaning the skin, inserting a needle, and delivering medication (such as anti-inflammatory steroids, lubricating fluid, or other therapeutics) – but the key difference is the imaging guidance that ensures the needle goes to the right place. By contrast, traditional “blind” injections rely only on feeling bony landmarks or using the clinician’s best guess of the target. Ultrasound guidance takes the guesswork out by letting the doctor see inside the joint during the injection, leading to much higher confidence that the medication is delivered where it’s needed.
Accuracy and Safety Advantages (Precise Placement, Avoiding Nerves)
One of the biggest benefits of ultrasound guidance is accuracy. Because the doctor can see the needle’s position and the anatomy in real time, the injection can be placed exactly into the joint space or around the tendon/area that requires treatment. This precise placement contrasts with blind injections, which can sometimes miss the target. In fact, studies have found that blind injections often have surprisingly low accuracy in certain joints. For example, a review noted that a particular shoulder joint injection (the acromioclavicular joint) hit the right spot only about 45% of the time when done without imaging – whereas with image guidance it was 100% accurate . With ultrasound, the doctor can also confirm that the medication spreads in the correct area immediately. Hitting the target on the first try means you’re more likely to get pain relief from that injection, rather than having a failed injection that provides little benefit.
Ultrasound guidance also improves safety during injections. Real-time imaging allows the clinician to avoid sensitive structures like nerves, blood vessels, and organs that might be near the injection site. In a blind injection, there’s a small risk that the needle could accidentally hit a nerve or blood vessel, potentially causing pain, bleeding, or other complications. Using ultrasound, the doctor can visualize these structures and steer clear of them, minimizing the risk of tissue damage or injection-related complications. This not only makes the procedure safer but often less painful as well – the needle isn’t poking around blindly, so there’s less trial-and-error that could irritate tissues. In fact, ultrasound-guided injections have been shown to cause less discomfort for patients during the procedure than blind injections, since the most accessible route can be chosen and nerves can be avoided. Overall, the accuracy and safety of ultrasound guidance give both the patient and doctor more confidence in the procedure.
Improved Outcomes and Pain Relief
Because ultrasound guidance ensures the medication is delivered to the precise location, patients often experience better outcomes from their injections. The whole point of a joint injection is to get the therapeutic substance (for example, a steroid or hyaluronic acid) into the exact area of inflammation or injury. If a blind injection misses and the drug is deposited outside the joint or in the wrong tissue, the patient might not feel much improvement. By increasing the accuracy, ultrasound guidance increases the likelihood that the injection will do its job – reducing pain and improving function in that joint.
Research supports that ultrasound-guided injections can lead to superior pain relief and functional recovery compared to blind injections. For instance, a systematic review of shoulder injections found that patients who received ultrasound-guided steroid injections had significantly greater improvement in shoulder pain and range of motion at 6 weeks post-injection than those who had landmark-guided injections. In other words, the guided injections were more effective in easing pain and restoring function. Similar trends have been observed for other joints and conditions: injections given with imaging tend to yield better clinical outcomes, especially in the early weeks following the injection, than their blind counterparts. Additionally, getting the injection right the first time may reduce the need for repeat injections or more invasive treatments down the line. Some practitioners also note that using ultrasound can make injections more cost-effective in the long run – even though the technique may involve a bit more setup, it can save patients from ineffective treatments and multiple doctor visits by getting results faster. Ultimately, for people suffering from joint pain, the goal is pain relief and return of mobility. Ultrasound-guided injections offer a higher chance of achieving that goal, as the medication is placed exactly where it needs to act.
Which Conditions Benefit Most from Ultrasound Guidance
Almost any joint injection can be improved with ultrasound guidance, but it’s particularly helpful for certain joints and conditions. In general, the more complex or small the joint, the more you gain from using imaging to guide the needle. Here are a few examples of conditions and areas that benefit greatly from ultrasound-guided injections:
• Shoulder Problems: The shoulder has multiple joint spaces and bursae that can cause pain (for example, a frozen shoulder or rotator cuff impingement). Guiding the needle via ultrasound ensures the medication (such as a steroid for a frozen shoulder) actually reaches the intended space. Ultrasound significantly improves accuracy for shoulder injections – some studies found landmark-only shoulder injections can be inaccurate about 20–55% of the time, whereas ultrasound guidance boosts accuracy to well over 90%. This precision can translate to better pain relief for conditions like adhesive capsulitis, bursitis, or arthritis in the shoulder.
• Knee Osteoarthritis: The knee is a large joint and somewhat easier to inject blindly than small joints, yet ultrasound can still be very beneficial. In cases of knee arthritis or chronic knee pain, an ultrasound-guided injection (whether it’s a corticosteroid or a viscosupplement gel) ensures the medication goes into the knee joint cavity rather than into surrounding soft tissue. This is especially useful if the joint spaces have narrowed (as often happens in arthritis) or if the patient has a complicated anatomy. Studies have shown that ultrasound-guided knee injections are over 95% accurate, essentially guaranteeing the treatment is delivered inside the joint where it can provide relief. Patients with knee osteoarthritis often report significant improvement in pain and mobility after a properly placed injection.
• Hip and Pelvic Joint Pain: The hip is a deep joint surrounded by thick muscles, making blind injections difficult. Using ultrasound (or sometimes X-ray guidance) for hip joint injections is standard practice to ensure the needle reaches the hip joint capsule. Conditions like hip osteoarthritis or trochanteric bursitis (inflammation of the bursa on the outer hip) benefit from guided injections because the target areas are small and not easily hit without imaging. Ultrasound guidance can also assist with injections around the pelvis, such as sacroiliac joint injections or piriformis syndrome injections, although some of these may require other imaging modalities. Guiding these injections with ultrasound improves accuracy and helps avoid the important nerves and blood vessels in the hip area.
• Ankle and Foot Conditions: The ankle and foot contain many small joints (like the ankle joint, subtalar joint, or the joints of the toes) and tight spaces that are hard to target blindly. For instance, an injection for ankle arthritis, plantar fasciitis, or a Morton’s neuroma in the foot can be done more confidently with ultrasound. With conditions such as Achilles tendonitis or plantar fasciitis, ultrasound helps guide the injection to the precise site of inflammation while avoiding nearby structures like the plantar nerves. By visualizing the foot/ankle anatomy, the clinician can ensure the medication (or platelet-rich plasma, etc., depending on treatment) goes exactly where intended. This can improve the effectiveness of injections for foot and ankle pain and reduce the risk of inadvertently hitting a tendon or nerve.
• Hand and Wrist Joints: Small joints in the hand, like the base of the thumb (carpometacarpal joint) or wrist joints, greatly benefit from ultrasound guidance. These tiny joints are notoriously tricky to inject with just landmark guidance. In fact, one study on thumb base arthritis found the accuracy of blind injections in that joint was only 38%, whereas using ultrasound raised it to 72% accuracy. Conditions such as thumb arthritis, wrist osteoarthritis, or tendon sheath inflammations (like De Quervain’s tenosynovitis) can be treated more effectively with guided injections. The ultrasound lets the doctor navigate the needle into small areas of the hand/wrist with millimeter precision, ensuring the medication bathes the affected tissue. Patients with hand or wrist pain (for example, from arthritis or carpal tunnel syndrome requiring a hydrodissection injection) often have better outcomes when these injections are done under ultrasound visualization.
In summary, while almost any joint pain condition can benefit from the added accuracy of ultrasound guidance, it is especially useful for complex joints (shoulder, hip), small joints (hand, wrist, foot), and situations where there are critical structures to avoid. Even for larger joints like the knee, many clinics in London and elsewhere now use ultrasound routinely to maximize the success of the injection.
Patient Experience: What to Expect During an Ultrasound-Guided Injection
If you’re considering an ultrasound-guided injection, you might be wondering what the actual procedure is like. The good news is that it’s usually a quick outpatient procedure, and knowing what to expect can help put you at ease. In general, an ultrasound-guided joint injection involves a few simple steps:
1. Preparation: You will either sit or lie down on an exam table, depending on which joint is being treated. The clinician will locate the target area using ultrasound gel and the probe, and may also mark your skin. Your skin will be cleaned with an antiseptic solution to prevent infection. For certain injections, a small amount of local anesthetic might be injected first to numb the skin and tissues, so that you feel minimal pain from the actual injection needle. The doctor will explain the procedure to you and you’ll have a chance to ask any last questions before you give consent.
2. Guided Injection Procedure: Once you’re prepped, the doctor (often a radiologist or sports medicine physician trained in ultrasound) will position the ultrasound transducer on your skin to visualize the joint. You’ll likely see the live image on a screen. They will then insert a thin needle through the numbed area and advance it toward the target, all while watching the needle’s progress on the ultrasound monitor. You might feel pressure or a mild sensation as the needle goes in, but because of the local anesthetic and the careful guidance, most patients report that it’s quite tolerable (often less painful than a typical blood draw). The doctor guides the needle tip into the exact spot needed – for example, into the joint capsule or adjacent to a tendon – and then injects the medication. Ultrasound visualization confirms that the medication spreads properly in the area. The whole injection process is usually very quick (a matter of seconds once the needle is in position). After injection, a small bandage may be placed over the needle entry point. The entire appointment typically takes only about 15–20 minutes in total, and then you’re done!
3. After the Injection: Right after the injection, you might notice the area feels a bit numb or “different” – that’s often due to the local anesthetic included in the injection, and it can cause temporary numbness or weakness around the joint for a few hours . Once the numbing wears off, your original pain may return initially. In some cases, people experience a slight increase in soreness for a day or two after the injection (this can happen, for example, with steroid injections known as a “cortisone flare”). Don’t be alarmed; this soreness usually settles within 48 hours. You can use mild pain relievers like paracetamol/acetaminophen or ibuprofen if needed for that initial post-injection soreness. The doctor may advise you to take it easy for the rest of the day (no intense exercise on that joint), but in most cases you can resume normal activities by the next day. Over the next couple of weeks, you should start to notice the therapeutic effects of the injection. Most people report improvement in their symptoms within 2–3 weeks after an ultrasound-guided injection. In favorable cases, relief can last for many months – and in some instances, the pain might not return at all if the underlying issue has resolved. Your doctor will likely schedule a follow-up or advise you on next steps, depending on the condition treated. They will also instruct you on any warning signs to watch for (for example, signs of infection are extremely rare, but you’d be told to look out for increasing redness, swelling, or fever and to report it if it happens). Fortunately, serious side effects are uncommon. Overall, patients often find that the procedure is quick and relatively comfortable, and they appreciate the peace of mind knowing the injection was placed accurately with ultrasound guidance.
Ultrasound-guided injections represent an exciting advance in joint pain treatment, giving patients a safer and more precise option for relief. The combination of real-time visualization, higher accuracy, and improved outcomes makes this technology a valuable tool for both doctors and patients. Whether you’re dealing with a stubborn shoulder pain or arthritic knees, ultrasound guidance can help ensure you get the maximum benefit from an injection therapy. Many clinics and hospitals (including those in London) now offer ultrasound-guided injections as a standard part of joint pain treatment technology. If joint pain is slowing you down, talk to your healthcare provider about whether an ultrasound-guided injection could be right for you. With its accuracy and safety advantages, it just might be the precise solution you need to get back on your feet with less pain.